Introduction
Type 2 diabetes presents a significant healthcare challenge globally, affecting millions of individuals and posing risks of various complications if not managed effectively. In this comprehensive guide, we delve into the multifaceted nature of type 2 diabetes, exploring its definition, management strategies, available medications, and other treatment options, and addressing frequently asked questions to provide a thorough understanding of this chronic condition.
Definition and Epidemiology of Type 2 Diabetes
Type 2 diabetes, characterized by elevated blood sugar levels resulting from either insufficient insulin production or the body’s inability to utilize insulin effectively, is a chronic metabolic disorder. While it can occur at any age, it is more prevalent in individuals over the age of 45, with the majority of cases developing after this age threshold. According to statistics, approximately 37 million people in the United States alone are diagnosed with diabetes, with type 2 diabetes accounting for 90–95% of cases.
Understanding Type 2 Diabetes: Mechanisms and Symptoms
Type 2 diabetes develops when the body’s cells become resistant to insulin or when the pancreas fails to produce enough insulin to meet the body’s needs. Insulin, a hormone produced by the pancreas, plays a crucial role in regulating blood sugar levels by facilitating the uptake of glucose into cells for energy production. When insulin resistance occurs, glucose accumulates in the bloodstream, leading to hyperglycemia. Common symptoms of type 2 diabetes include frequent urination, increased thirst and hunger, fatigue, blurred vision, and unexplained weight loss.
Management Strategies for Type 2 Diabetes
Effectively managing type 2 diabetes is essential for preventing complications and improving overall health outcomes. A comprehensive approach to management includes the following strategies:
- Dietary Modifications: Adopting a balanced, nutritious diet low in refined sugars and carbohydrates can help regulate blood sugar levels. Emphasis should be placed on consuming whole grains, fruits, vegetables, lean proteins, and healthy fats while limiting intake of processed foods and sugary beverages.
- Physical Activity: Regular exercise is beneficial for improving insulin sensitivity, lowering blood sugar levels, and promoting weight loss. Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity per week, along with muscle-strengthening exercises on two or more days per week.
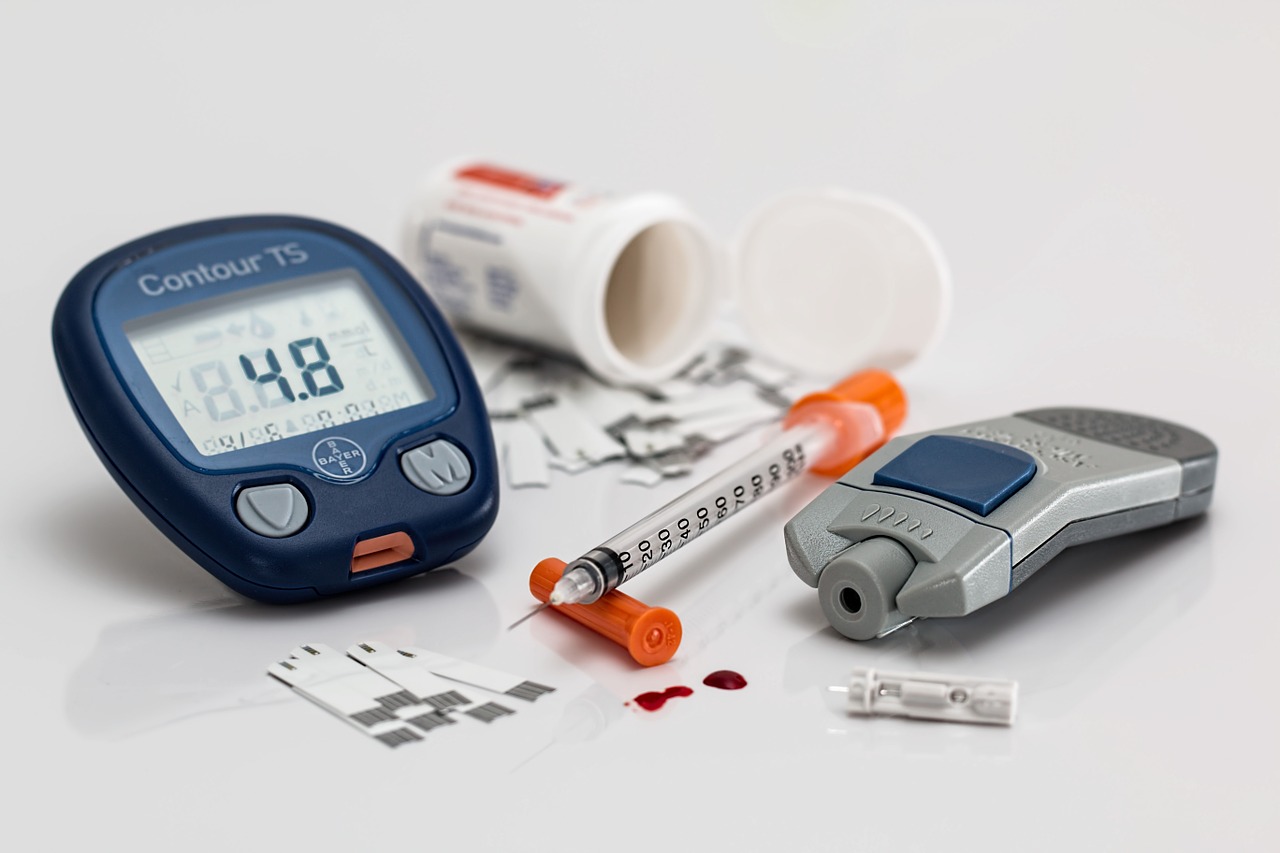
- Blood Glucose Monitoring: Regular monitoring of blood sugar levels allows individuals to track their condition’s progression and make necessary adjustments to their treatment plan. Self-monitoring devices, such as glucometers, provide valuable insights into daily blood sugar fluctuations.
- Stress Management: Chronic stress can negatively impact blood sugar control. Implementing stress-reduction techniques such as mindfulness, meditation, yoga, and deep breathing exercises can help mitigate stress levels and improve overall well-being.
- Medication Management: Depending on individual needs and disease progression, healthcare providers may prescribe various medications to help manage blood sugar levels effectively. These medications include oral hypoglycemic agents, injectable insulin, and other adjunctive therapies.
Medications for Type 2 Diabetes
Several classes of medications are available to treat type 2 diabetes, each with its unique mechanism of action and benefits. These medications include:
- Alpha-Glucosidase Inhibitors (AGIs): AGIs slow down the absorption of carbohydrates from the small intestine, reducing postprandial blood sugar spikes. Common examples include acarbose and miglitol.
- Biguanides: Biguanides, such as metformin, decrease liver sugar production, enhance insulin sensitivity, and reduce intestinal sugar absorption, thereby lowering blood sugar levels.
- Dopamine Agonists: Originally used to treat Parkinson’s disease, dopamine agonists may also aid in blood sugar regulation. Bromocriptine is a commonly prescribed dopamine agonist for type 2 diabetes management.
- Dipeptidyl Peptidase-4 (DPP-4) Inhibitors: DPP-4 inhibitors enhance insulin secretion and decrease glucagon production, helping to lower blood sugar levels. Examples include sitagliptin, saxagliptin, and linagliptin.
- Glucagon-Like Peptide-1 (GLP-1) Receptor Agonists: GLP-1 receptor agonists stimulate insulin secretion, inhibit glucagon production, and promote weight loss. These medications are available in both injectable and oral formulations, with examples including exenatide, liraglutide, and dulaglutide.
- Meglitinides: Meglitinides stimulate insulin production, particularly after meals, to help control postprandial blood sugar levels. Examples include repaglinide and nateglinide.
- Sodium-Glucose Transporter 2 (SGLT2) Inhibitors: SGLT2 inhibitors reduce glucose reabsorption by the kidneys, promoting its excretion via urine. Canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin are commonly prescribed SGLT2 inhibitors.
- Sulfonylureas: Sulfonylureas stimulate insulin secretion from the pancreatic beta cells, helping to lower blood sugar levels. Examples include glimepiride, glipizide, and glyburide.
- Thiazolidinediones (TZDs): TZDs enhance insulin action and increase insulin sensitivity, thereby improving blood sugar control. Common examples include pioglitazone and rosiglitazone.
Other Treatment Options
In addition to medication, individuals with type 2 diabetes may require insulin therapy or weight loss surgery, particularly if obesity is present. Insulin therapy may be administered via various methods, including insulin pens, pumps, inhalers, or jet injectors, depending on individual needs and preferences. Weight loss surgery, such as gastric bypass or sleeve gastrectomy, may be recommended for individuals with severe obesity and uncontrolled diabetes.
Maintaining a Healthy Lifestyle
A holistic approach to managing type 2 diabetes involves adopting healthy lifestyle habits that promote overall well-being. These include:
- Healthy Eating: Consuming a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting processed foods, sugary snacks, and beverages.
- Regular Exercise: Engaging in regular physical activity, including aerobic exercises, strength training, and flexibility exercises, to improve insulin sensitivity, lower blood sugar levels, and promote weight loss.
- Stress Reduction: Practicing stress-reduction techniques such as mindfulness, meditation, yoga, and deep breathing exercises to alleviate stress and improve mental well-being.
- Smoking Cessation: Quitting smoking is essential for individuals with type 2 diabetes, as smoking can exacerbate cardiovascular complications and impair blood sugar control.
When to Seek Medical Assistance
Persistent side effects or severe reactions to diabetes medications warrant immediate medical attention. Additionally, individuals experiencing symptoms such as severe hyperglycemia (high blood sugar), hypoglycemia (low blood sugar), diabetic ketoacidosis, or hyperosmolar hyperglycemic state should seek prompt medical assistance to prevent complications.
Outlook
While type 2 diabetes is a chronic condition without a cure, effective management strategies, including lifestyle modifications, medication interventions, and regular medical monitoring, can significantly improve
Frequently Asked Questions (FAQs)
1. How should I manage diabetes if I’m pregnant?
Managing diabetes during pregnancy requires specialized care to ensure the health and well-being of both the mother and the baby. Pregnant individuals with type 2 diabetes should work closely with their healthcare team, including obstetricians, endocrinologists, and diabetes educators, to develop a comprehensive treatment plan. This plan may include regular monitoring of blood sugar levels, adjustments to diet and exercise routines, and, in some cases, medication management. It’s essential to attend all prenatal appointments and follow medical recommendations to reduce the risk of complications such as fetal development abnormalities, cesarean delivery, preeclampsia, early birth, low blood sugar, miscarriage, and stillbirth.
2. What is the safest type 2 diabetes medication for people with kidney disease?
Individuals with type 2 diabetes and kidney disease require careful consideration when selecting diabetes medications, as some medications may exacerbate kidney function decline. Metformin is often considered the first-line medication for managing type 2 diabetes in individuals with kidney disease, as it is safe and effective in this population. However, dosage adjustments may be necessary based on the individual’s kidney function. Other diabetes medications, such as certain sulfonylureas and DPP-4 inhibitors, may also be suitable for individuals with kidney disease, depending on their specific medical history and kidney function. It’s essential to consult with a healthcare professional to determine the most appropriate treatment plan tailored to the individual’s needs and medical condition.
3. Can type 2 diabetes be reversed through lifestyle changes?
While type 2 diabetes is a chronic condition that cannot be cured, lifestyle changes, including diet, exercise, and weight management, can play a significant role in managing the disease and improving overall health outcomes. Research has shown that adopting a healthy lifestyle, such as following a balanced diet, engaging in regular physical activity, maintaining a moderate weight, and avoiding tobacco use, can help control blood sugar levels, reduce the risk of complications, and improve the quality of life for individuals with type 2 diabetes. In some cases, significant weight loss achieved through lifestyle changes may even lead to remission of type 2 diabetes, where blood sugar levels return to normal without the need for medication. However, it’s essential to work closely with healthcare professionals to develop a personalized treatment plan and monitor progress regularly.
4. Are there any natural remedies or supplements that can help manage type 2 diabetes?
While some natural remedies and dietary supplements have been purported to help manage type 2 diabetes, it’s essential to approach these with caution and consult with a healthcare professional before incorporating them into your treatment plan. Some supplements, such as chromium, alpha-lipoic acid, and cinnamon, have shown potential in improving insulin sensitivity and blood sugar control in some studies. Additionally, certain herbal remedies, such as bitter melon, fenugreek, and ginseng, have been used traditionally to help manage diabetes symptoms. However, the evidence supporting the effectiveness and safety of these supplements in managing type 2 diabetes is limited, and more research is needed to validate their use. It’s crucial to discuss any supplements or natural remedies with your healthcare provider to ensure they are safe and appropriate for your individual needs and medical condition, as they may interact with medications or have adverse effects.
5. What are the long-term complications of uncontrolled type 2 diabetes?
Uncontrolled type 2 diabetes can lead to a variety of long-term complications affecting various organs and systems in the body. These complications may include cardiovascular disease, neuropathy (nerve damage), nephropathy (kidney disease), retinopathy (eye damage), foot complications (such as ulcers and infections), skin conditions, hearing impairment, and cognitive decline. Additionally, individuals with uncontrolled diabetes may be at increased risk of developing other health problems, such as high blood pressure, high cholesterol, and sleep apnea. Managing blood sugar levels and following a comprehensive treatment plan can help reduce the risk of complications and improve overall health outcomes for individuals with type 2 diabetes. Regular medical monitoring and preventive care are essential for early detection and management of potential complications.
Read our previous article: The Comprehensive Guide to Blood Sugar Regulation: Insights into Insulin, Glucagon, and Metabolic Harmony
Sports Update: These medications are available in both injectable and oral formulations, with examples including exenatide, liraglutide, and dulaglutide Stay tuned for more updates on Comprehensive Guide to Managing Type 2 Diabetes: Strategies, Medications, and FAQs and other trending sports news!
Your Thoughts Matter! What’s your opinion on Comprehensive Guide to Managing Type 2 Diabetes: Strategies, Medications, and FAQs? Share your thoughts in the comments below and join the discussion!